Specializing in Pelvic Floor Rehabilitation, Pelvic Pain, Pregnancy & Postpartum Care
What is Women's Health & Pelvic Floor Physical Therapy?
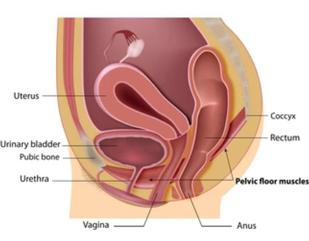
Women’s health physical therapists, also known as pelvic floor physical therapists, treat a variety of problems, but they are most well known for their treatment of pelvic floor dysfunction. The pelvic floor muscles, located in the perineum, are responsible for bowel, bladder and sexual function in addition to their role as a stabilizer or a “core” muscle. There are two main categories of pelvic floor dysfunction: "underactive (weak) pelvic floor muscles" and "overactive (tight) pelvic floor muscles."
Women with weak pelvic floor muscles may experience:
• Urinary Incontinence
• Fecal Incontinence and/or Flatulence
• Pelvic Organ Prolapse (Dropped Uterus, Bladder Or Rectum)
• Discomfort or Pressure in the Pelvic or Vaginal Area that may or may not Interfere with Intercourse
• Difficulty Fully Emptying Bladder
• Decreased Libido and/ or Decreased Sexual Response
Risk Factors for weak pelvic floor muscles include:
• Pregnancy (risk increases with each pregnancy)
• Vaginal Delivery, even greater with
o Pushing for more than 2 hours
o Episiotomy or Large Perineal Tears
o Forceps or Vacuum Assisted Delivery
o Large birth weight of baby
• Constipation – straining to evacuate stool
• Chronic Coughing or Sneezing
• Menopause – muscle mass decreases with age and decreased estrogen causes thinning of vaginal tissue
• Gynecologic Surgery
• Obesity – the pelvic floor muscles have to work harder
• Excessive High Impact Exercise – increased symptoms shown in certain athletes
• Lack of Pelvic Floor Exercise - “use it or lose it”
Women with tight pelvic floor muscles may experience:
• Dyspareunia (pain with intercourse)
• Unconsummated Marriage
• Vaginal Pain syndromes including:
o Vaginismus
o Vulvodynia
o Vestibulitis
• Urinary Urgency and Frequency
• Chronic Constipation
Physical therapy can also ease symptoms of various pelvic pain syndromes by relaxing tight pelvic floor muscles and/ or by improving muscle balance throughout the body. This includes:
• Interstitial Cystitis
• Endometriosis
• Painful Bladder Syndrome
• Irritable Bowel Syndrome
• Chronic Pelvic Pain Syndrome
• Pudendal Neuralgia
• Coccydynia (tailbone pain)
Very often, women with these kinds of problems try various medications or other methods with little relief and may be facing surgery. Two reasons for this are that:
1) According to research studies, 50% of women who are told to "do kegels" by their doctor are doing them incorrectly and therefore they need more help.
2) Pelvic and vaginal pain syndromes are poorly understood in the medical community, therefore many women have trouble finding the help they need. Many women see several doctors before learning about physical therapy. Physical therapy may avoid the need for medications and surgery for many patients. For others, the physical therapist may act as a liaison in helping the patient receive the medical care that they need.
Women’s health physical therapists also specialize in the treatment of women during the pregnancy and postpartum period. During pregnancy, the physical therapist works to make the pregnant woman more comfortable and functional by resolving or managing conditions such as:
• Low Back Pain
• Sciatica
• Sacroiliac Joint Dysfunction
• Pubic Symphysis Pain and/ or Separation
• Coccydynia (tailbone pain)
• Carpal Tunnel Syndrome
• Thoracic Outlet Syndrome
• Upper back pain
• Neck Pain
• Headaches
• Hip Pain
• Urinary incontinence
• Vaginal Pain
Physical therapy during the latter months of pregnancy may promote a smooth vaginal delivery by correcting pelvic and spinal alignment and increasing the mother’s flexibility.
Postpartum, the physical therapist may manage the same conditions listed above in addition to:
• Scar Pain (cesarean, episiotomy, perineal stitches)
• Diastasis Recti
• Urinary and Fecal Incontinence
• Pelvic Organ Prolapse
• Clogged Milk Ducts
Dr. Rivka Friedman will provide you with a thorough initial evaluation which includes:
• A detailed medical history and history of your problem
• An orthopedic exam to assess joint function and mobility, muscle flexibility, muscle strength, nerve function and special tests to check for specific conditions
• A pelvic floor exam to assess skin condition, nerve function, muscle pain, muscle strength, tissue integrity and testing for pelvic organ prolapse
• A detailed explanation of your condition and the treatment plan
Your treatment may include:
• Manual Therapy techniques such as
o Myofascial Release
o Visceral (organ) Mobilization/ Abdominal Massage
o Various Massage Techniques
o Scar Mobilization Techniques
o Joint Mobilization and Alignment Correction
o Nerve Mobilization Techniques
o Muscle Relaxation/ Stretching Techniques
• Neuromuscular Re-Education techniques to enhance muscle performance and function
• Electrical Modalities such as
o Biofeedback
o Electrical Stimulation
o Ultrasound
• An individualized Home Exercise Program to improve joint mobility, muscle flexibility, strength and to decrease pain
Just like women need to go to their doctor for annual gynecologic exams and mammograms, I highly recommend that all women have a wellness check of their pelvic floor. This can promote early detection and treatment of the above listed conditions. Like other illnesses, these conditions are much easier to treat in the early stages.
© 2024 Dr. Rivka Friedman Physical Therapy for Women, LLC
(954) 399-3241